One evening as I was using my key to let myself into my mother’s apartment for a visit, I glanced toward the kitchen table where she usually sat reading the newspaper and saw her rolling walker standing alone. Surprised, I said loudly: “Where are you, Mom?”
“Here,” I heard her respond from her bedroom down the hall. “I’m fine.”
On the floor next to her bed, I found her splayed out on her back. “Did you fall? Are you hurt?” I asked with rising panic.
“I’m fine,” she repeated. “It’s comfortable here,” she said, running her hand lightly over the cut-pile carpet.
My thoughts went in several directions. As a clinical psychologist specializing in working with older adults and their family caregivers for two decades, I’d heard many stories of seniors lying where they’d fallen for hours or even days before being found. Why hadn’t she used her walker to prevent her fall? She hated it, I knew, because it made her feel old, but a botched knee replacement surgery and bad arthritis had made her gait unsteady. Had she forgotten it in her kitchen because her thinking skills were declining, or decided to not use it when no one – ie, me – was watching?
“How long have you been here?” I asked as I lifted her gently and guided her to a chair.
“A little while,” she answered. I didn’t believe her.
“Why didn’t you use the medical alert?” I asked, pointing to the button she had on a necklace around her neck which, when pushed, would connect her to an emergency service.
She fingered the necklace but said nothing. Had she forgotten about it, too, I wondered, or had she decided not to use it out of embarrassment?
Such concerns about an older adult are increasingly common in our ageing America. According to the 2025 Caregiving in the US report, published in July by AARP and the National Alliance for Caregiving, nearly half of this country’s 63 million family caregivers are caring for their ageing or disabled parents. Many of these adult children, the report makes clear, are overwhelmed by the number and nature of caregiving tasks, such as driving their parents to medical appointments, managing their bills, and even dressing, bathing and toileting them. Because many of these children cut back on their work hours to be available to provide care, they frequently develop financial problems. Many feel unsupported by friends, other family members and employers as they try to do the right thing for their parents.
The report misses a key caregiving challenge, however. In my professional and personal experience, it is the relationship between parent and child that largely determines whether their caregiving experience is hard, but gratifying or full of conflict and regret. Too often during caregiving, that parent-child bond is severely stressed by pride, minimization and resistance.
What happened between my mother and me exemplified this. She was deservedly proud – a poor Bronx girl and child of Polish-Jewish immigrants who was her high school valedictorian and a stellar student at City College of New York. She had worked hard as a teacher, had run a successful insurance brokerage and had led several community organizations. Throughout her adult life, she’d constructed a self-identity as a smart striver who overcame long odds to go far, including traveling extensively on five continents.
But as she became frail and forgetful with age, her pride became a problem. She hated being in the position of needing help and accepted it only grudgingly, especially from me, her oldest son. I’d heard many caregiving clients over the years report that their “stubborn” parents were reluctant to allow them to assist them for fear of being a burden. My mother felt all this and more. It was as if the idea that I’d be her caregiver and she’d be my care receiver seemed to her an abhorrent reversal of the parent-child hierarchy.
She protected her pride by using minimization, a close cousin of denial. It wasn’t that she refused to believe she had kidney disease from chronically high blood pressure or that a car accident years ago and physical wear-and-tear caused her marked back and knee pain, but she made light of their impact on her capabilities. In her mind, she didn’t really need her walker nor a commode atop her toilet nor a notebook to write things down to remember them. She could still manage to drive safely, she was convinced, despite my contention otherwise.
Most of us use the psychological mechanism of minimization by choosing to believe that our faults are not so onerous and that we are better than we probably are. With older adults, however, minimization may also have roots in neurology. A common early symptom of dementia is “anosognosia” or an inability to appreciate one’s physical or cognitive deficits. The same chronically high blood pressure negatively affecting my mother’s kidneys was also slowly damaging her brain. It took years for her to be diagnosed with vascular dementia. That almost certainly amplified her tendency to minimize.
Pride plus minimization leads to resistance. There was almost nothing I could recommend to my mother that she didn’t initially reject. She resisted my efforts to hire personal care aides or get home-delivered meals for her. She balked at my suggestion to economize to stretch her paltry savings. She was furious when I took control of organizing her pill box.
Like most adult-child caregivers, I wanted to preserve my mother’s dignity while ensuring her safety. I took the same approach I’d counseled many caregiving clients of ageing parents. I tried to lead with empathy for the losses she was experiencing by recognizing that she was often in pain and telling her that I admired how she was still doing the best she could. I told her I wanted to be her ally, not adversary, in helping her live as she preferred to whatever degree possible and that I wanted to support her, not overrule her, with most of the decisions she made. When I did need to overrule her at times, telling her it was unsafe for her to drive or manage her medications on her own, I tried to be as gentle as I could, while also reassuring her that I would take her where she wanted to go and manage her medicines for her. If my mother fought back, however, it wasn’t always possible for me to be gentle; I insisted on changes I felt she needed.
As my mother continued to decline over time, her pride was hurt further and she minimized less as her deficits became more glaring. In one year, she had multiple broken bones, three hospitalizations and long rehab stays following a series of falls, including being found down one evening by a stranger in the parking lot of her apartment building. However, she never stopped resisting me. I was the villain who had curbed her independence and lorded power over her. “You are not my boss,” she told me in anger dozens of times.
I didn’t want to be her boss, I protested defensively. But the more I tried to explain the reasons for hiring the aides and getting the home-delivered meals, the more she resisted me. We were often at odds. I met her anger about being mistreated with my own anger about being miscast.
The tension between us made caregiving much harder for me. I felt angry, then guilty about having felt anger, then angry again about having been made to feel guilty. I had more reflective moments, though, too. I’d think back to the time I found her on the carpet. Was she really unfazed about being down, I considered in hindsight, or was that just bravado? Was the look in her eye as I lifted her up one of disbelief that she had fallen or was she rightfully frightened that she’d fall again? If I could see her resentment toward me as fear at her growing helplessness, then I could respond to her with empathy and not my own resentment at her resistance. When I was empathic, she argued less and agreed to disagree about the care I would arrange for her. Things became a little calmer between us.
Few of us adult children aspire to dominating our moms and dads. We want instead to be recognized by them and even thanked occasionally for acting responsibly. For that to happen, we need to think first about how their losses are impacting our relationships with them. We need to drive, feed and perhaps dress them but tend with great attention to their fears. We need to set aside anger and react less to become more aware and effective caregivers.
-
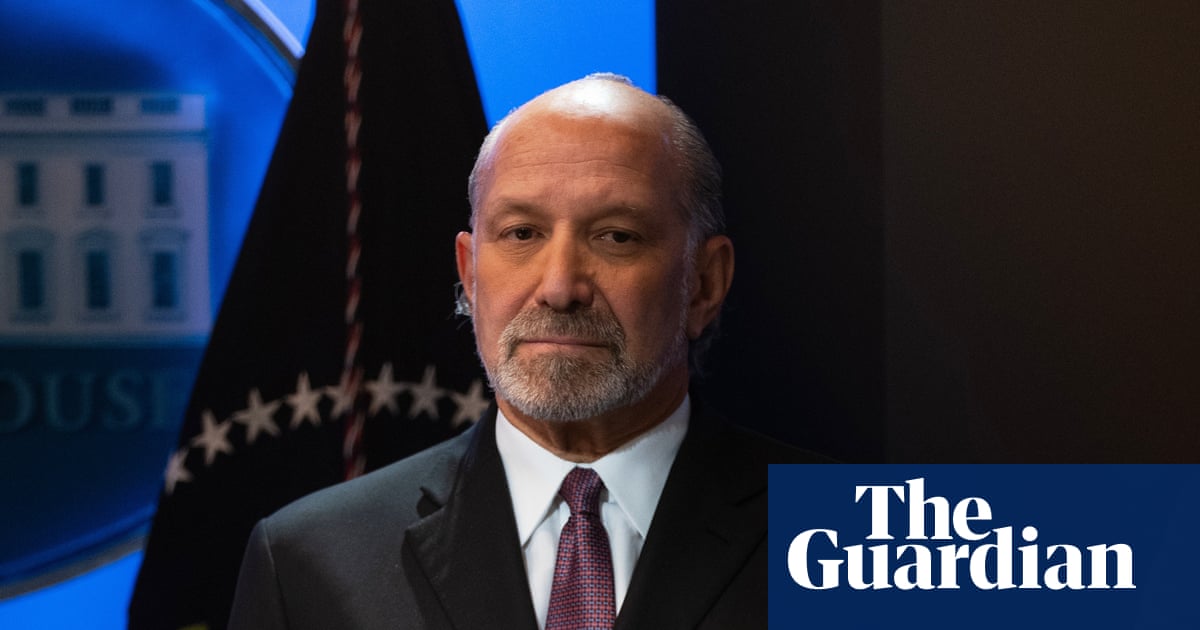
Barry J Jacobs, Psy D, is a Philadelphia-area clinical psychologist and author or co-author of three self-help books for family caregivers, including The AARP Caregiver Answer Book

 3 months ago
99
3 months ago
99