Tens of thousands of prescriptions have been issued in England for a promising and non-addictive new sleeping pill, but doctors say NHS uptake is being held back by cost and patchy awareness.
Daridorexant, approved last year, has been prescribed 67,000 times since November 2023, at an estimated cost of £2.6m to the NHS. The drug has been hailed for helping people fall asleep faster, stay asleep longer and wake up clear-headed – without the dependency risks of traditional pills.
But access is uneven. Prescribing is clustered in parts of London and the West Midlands, while some patients are turning to private care. By contrast, zopiclone – a far cheaper and potentially addictive alternative – was issued more than 7m times over the same period between November 2023 and June 2025. Nice had forecast the NHS would spend £10.9m on daridorexant in the financial year 2024-25, but costs so far are much lower, about £1.5m.
Doctors also caution against seeing it as a magic bullet solution; while many patients see improvements, a sizeable minority do not. As with all drugs there are side-effects.
Nice said 995,000 adults with insomnia were eligible for treatment with daridorexant based on expected population growth. They estimated 116,600 adults would start treatment with the drug in 2027-28 after adjusting for expected population growth.
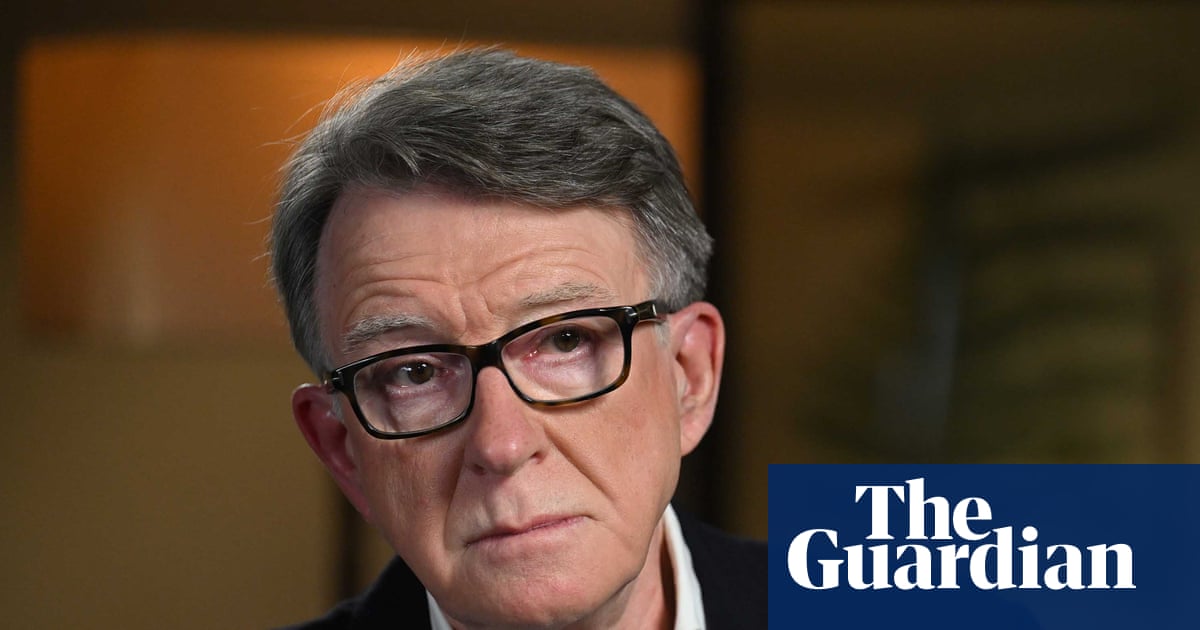
Prof Guy Leschziner, a consultant neurologist and leading sleep expert, called the drug “a significant step forward”. He said: “Unlike traditional sleeping pills, this drug carries a low risk of dependency and does not cause rebound insomnia when stopped. Concerns have been raised about older sleeping tablets and long-term cognitive decline, but at present we don’t see that risk with daridorexant.”
But he said the nature of prescription was cautious by design. He said: “Doctors are urged to prioritise CBT-I (cognitive behavioural therapy for insomnia), so tablets are only used if therapy fails, isn’t available or isn’t suitable. The problem is that access to CBT-I on the NHS is patchy, so many patients fall through the cracks.”
Cost is another sticking point. “Fourteen tablets of zopiclone cost the NHS 82p, compared with around £42 for 30 daridorexant tablets,” said Leschziner. “It’s far easier to access privately, but within the NHS, hospitals bear the cost when specialists prescribe it – and that money has to be found from elsewhere in already stretched budgets.”
Daridorexant works by blocking orexin receptors, which drive wakefulness, so instead of forcing sedation like benzodiazepines, it simply removes the “stay awake” signal.
Side-effects of daridorexant include headache, sleepiness or fatigue, dizziness and nausea. Less commonly, it may affect mood, cause abnormal dreams, or worsen depression in susceptible patients.
Prof Colin Espie, an Oxford sleep medicine expert, said uptake had been slower than Nice predicted, though prescribing is now growing at about 12% a month.
But he said: “What’s more pressing is the continued lack of access to the first-line treatment for insomnia, CBT-I. Access to second-line options like daridorexant matters, but patients deserve the most evidence-based care – and in this condition, that means therapy, not tablets.”
Dr Alanna Hare, the president of the British Sleep Society, said there was “always a lag” when new drugs were rolled out, though work was under way to raise awareness.
She said cost-effectiveness had already been demonstrated in Nice’s appraisal, adding: “Daridorexant improves sleep by cutting night-time waking by about 20 minutes and sleep onset by 12 minutes, but more importantly, it boosts people’s perception of sleep quality and their daytime functioning.”
She stressed that CBT-I remained the most effective treatment, benefiting about 80% of patients. “Even brief behavioural interventions can work, and digital platforms like Sleepio and Sleepstation are vital to delivering CBT-I at scale,” she said. “Daridorexant should be seen as complementary to, not a replacement for, therapy.”
Leschziner said that while the “majority of patients see improvements with daridorexant”, it does not work for “a sizeable minority”. He said: “Expectations should therefore remain realistic, as it is not a wonder drug.”

 3 months ago
94
3 months ago
94