One in seven people in England who need hospital care are not receiving it because their GP referral is lost, rejected or delayed, the NHS’s patient watchdog has found.
Three-quarters (75%) of those trapped in this “referrals black hole” suffer harm to their physical or mental health as a result of not being added to the waiting list for tests or treatment.
Communication with patients is so unreliable that seven in 10 (70%) only discover they have not been put on a waiting list after chasing up the NHS because they have not been told a hold-up has occurred. In some cases referrals that GPs have agreed to make do not even get sent from their surgery to the hospital, Healthwatch England’s findings show.
The research found that 14% of all referrals are getting “stuck” between GPs and hospitals, leaving patients in the dark and anxious about when they will be seen and treated.
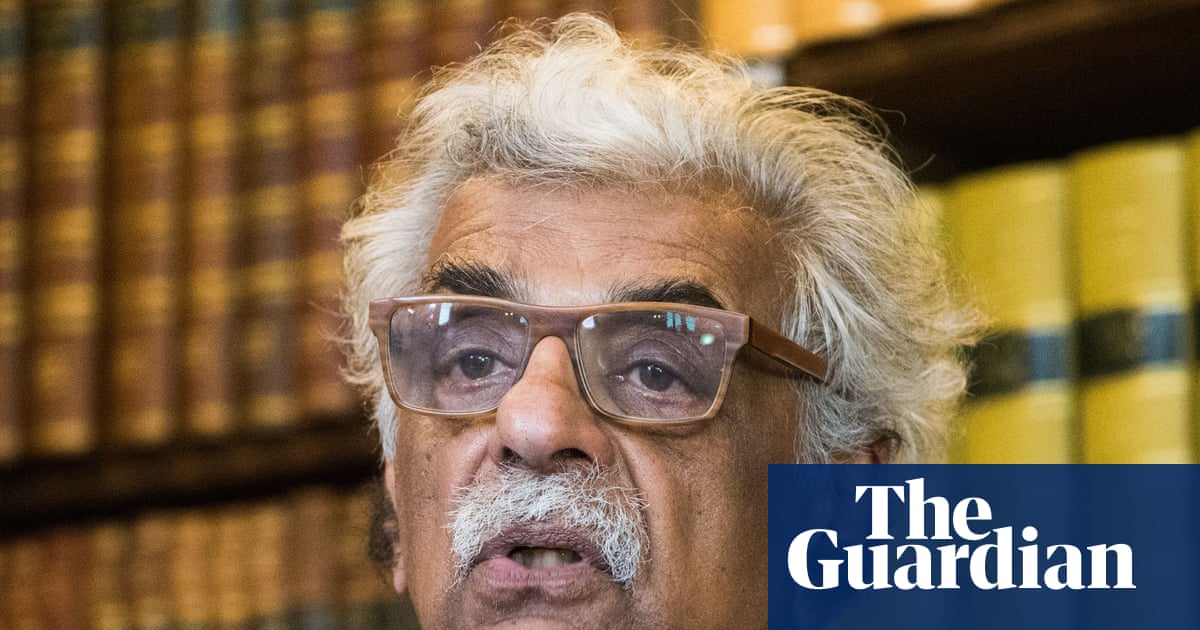
Chris McCann, Healthwatch’s deputy chief executive, said: “Behind every delayed, lost or rejected referral is a human story of pain, stress and uncertainty.
“While improvements have been made, too many people remain stuck in this referral ‘black hole’, telling us that they’re ‘existing not living’ due to delays.”
Rachel Power, the chief executive of the Patients Association, said the findings were “deeply alarming” and that delays to referrals can leave some patients afraid to leave their home.
“When seven out of 10 people only find out their referral failed because they chased it up themselves, something is badly wrong.
“These are people already anxious about their health, already stressed waiting for treatment – and then they discover they weren’t even in the queue. While they wait, their conditions could be getting worse,” said Power.
Healthwatch’s findings are based on a YouGov survey of a nationally representative sample of 2,622 adults in England whom a GP had referred for tests or treatment in the last year.
They raise questions about how accurate the NHS waiting list is as a true reflection of the number of people who need care – 6.24 million people are waiting for 7.39 million tests or treatments – and how good the service is at keeping patients informed about the progress of their referral.
Just over half (53%) of people referred seek medical help or advice while they wait for the NHS to act, the survey found. While 7% go private, one in five (20%) asks for help from other parts of the NHS, such as a different GP or urgent care services. “These results suggest that referral delays may increase pressure on other NHS services”, the report noted.
after newsletter promotion
One patient – Patrick, 70, an ex-NHS worker from Milton Keynes – told the watchdog how he had been waiting since July to see a specialist about pain in his hip and back.
After his GP referred him he heard nothing about when he would be seen. He said: “When I rang they were nice on the phone but they couldn’t give me any good news. It could be as long as a year before I get an appointment, and that’s just to take the first step in a long process.”
His pain has become so bad he struggles with daily tasks such as shopping, driving or even putting on his shoes. He does not know when he will be seen.
“I feel like I’m stuck in limbo,” he added.
The 14% of people whose referral gets lost, rejected or denied is an improvement on the 21% who experienced the same fate when the watchdog undertook similar research in 2023.
Since then ministers and health service chiefs have tried to tackle the problem by making it easier for patients to track the progress of their referral via the NHS app and using pharmacies to help people with suspected cancer.
“Yet, despite progress, many patients still report that poor communication, delays and uncertainty caused by long waits are affecting their health, wellbeing and ability to work,” Healthwatch said.
One in four (23%) people are dissatisfied with the referrals process, it found. Public satisfaction with the NHS generally has fallen to just 21% – the lowest level – the most recent British Social Attitudes survey found.
A Department of Health and Social Care (DHSC) spokesperson said the situation revealed by the findings was “not acceptable”. But improvements have been made since the research was done in March, the spokesperson added.
They include the introduction in September of Jess’s rule, under which GPs are meant to seek a second opinion if they cannot diagnose a patient’s illness after three appointments.
The DHSC is putting an extra £1.1bn into general practice, recruiting more family doctors and cutting red tape so GPs can spend more time with patients, the spokesperson added.
Family doctors are also now encouraged to seek “advice and guidance” from specialist hospital doctors about referrals. Patient satisfaction with primary care has risen from 60% in July 2024 to 75%.
The DHSC spokesperson said: “We have been clear that it will take time to turn around the NHS but we are starting to see improvements. There’s still a long way to go but we are beginning to see the green shoots of recovery.”

 1 month ago
75
1 month ago
75